Background:
Insufficient data exists on COVID-19 risks and hospitalization outcomes in patients with immune thrombocytopenia (ITP). Our analysis aims to assess risks and outcomes associated with COVID-19 in ITP patients.
Method:
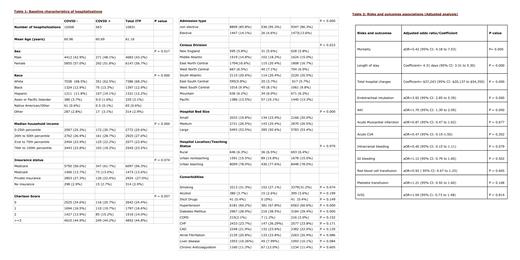
In this retrospective study, we obtained data from the National Inpatient Sample (NIS) database for the year 2020. Hospitalizations for ITP were identified using ICD-10 codes, further classified into those with and without COVID-19 infection (Table 1). To account for potential confounding factors, we considered variables such as age, sex, race, zip code-based income quartile, hospital region, hospital teaching status, hospital division, hospital bed size, and insurance status. Additionally, the Charlson index and relevant comorbid conditions such as smoking, alcohol use, illicit drug use, hypertension, diabetes mellitus, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease (CAD), atrial fibrillation (AF), liver disease, and chronic use of anticoagulants were included.
Firstly, univariable logistic regression analysis calculated unadjusted odds ratios (ORs). Then, to adjust for potential confounders, a multivariable logistic regression analysis was performed to calculate adjusted odds ratios (aORs) (Table 2). The multivariable logistic regression model only included variables associated with the outcome of interest in univariable regression analysis at P < 0.1. Proportions were compared using the Fisher exact test, and continuous variables were compared using the Student t-test. All P-values were two-sided, with a significance threshold of .05.
Results:
Data from 10,831 hospitalizations for ITP in 2020 were gathered. Among those, 563 hospitalizations were of patients with COVID-19. Unadjusted data revealed minimal differences in the mean age between both groups, but there was a statistical difference between COVID-positive and COVID-negative males (48.2% vs. 42.9%) and females (51.8% vs. 57.0%). White race had the highest number of patients in both groups with a statistical difference of 62.5% vs. 68.5%, p=0.000 compared to other races. Moreover, COVID-positive patients with ITP had a significantly higher rate of comorbidities like hypertension (67.8% vs. 60.2%, p=0.000) and diabetes mellitus (38.5% vs. 28.9%, p=0.000). On the other hand, there was no statistical difference between groups with associated comorbidities like smoking, alcohol, illicit drugs, COPD, CHF, CAD, atrial fibrillation, liver disease, and chronic anticoagulation use.
ITP patients with COVID-19 showed a significantly longer median length of stay (10.7 days vs. 6.3 days; p=0.000) and higher overall cost-of-hospitalization ($136,915 vs. $98,657; p=0.000). After adjusting for potential confounders using multivariate logistic regression, we found that ITP patients with COVID-19 had notably higher odds of mortality (adjusted odds ratio (aOR) = 5.42, 95% CI: 4.18 to 7.03, p=0.000), longer hospital stays (Coefficient: 4.31 days, 95% CI: 3.31 to 5.30, p=0.000), and increased total hospital charges (Coefficient: $37,243, 95% CI: $20,137 to $54,350, p=0.000). However, there were no statistically significant differences in the administration of PRBC transfusions, platelet transfusions, or immunoglobulin transfusions between the two groups. Additionally, no notable distinctions in the odds ratio of experiencing intracranial bleeding, gastrointestinal (GI) bleeding, myocardial infarction (MI), or acute cerebrovascular accident (CVA) were observed between ITP patients with and without COVID-19.
Conclusion:
In conclusion, this study highlights the higher risks and poorer hospitalization outcomes associated with COVID-19 in patients with immune thrombocytopenic purpura. The results of our study highlight the significance of taking COVID-19 infection into account when managing and evaluating outcomes in ITP patients, as it seems to be linked to more severe disease manifestations and higher utilization of healthcare resources. Further research and prospective studies are necessary to gain a deeper understanding and address the implications of COVID-19 in this particular patient population.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal